Inflammatory and spinal disorders primarily involve rheumatoid arthritis, ankylosing spondylitis and DISH and OPLL and ossification of the ligamentum flavum. We will focus on diagnosis, modern surgical techniques and outcomes.
Spinal disorders often have multiple etiologies (causes). Inflammatory disorders are one of multiple different etiologies including degenerative trauma, deformity, tumor and congenital abnormalities. Also grouped in inflammatory disorders are lupus, psoriasis, inflammatory bowel disease, gout and calcium pyrophosphate disease. We will focus on the ones previously mentioned.
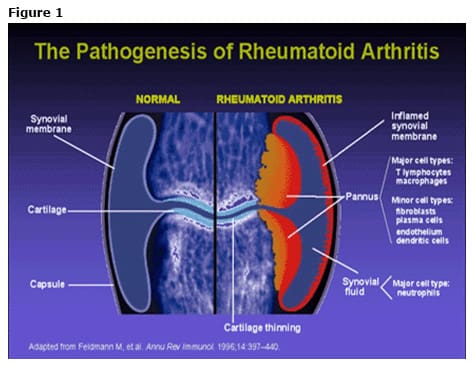
Rheumatoid arthritis is a symmetric inflammatory peripheral polyarthritis characterized as a Type III hypersensitivity reaction. It has a 1% prevalence higher in Native Indian populations and an unknown etiology but genetic risk factors have been associated with HLA genes. Protective factors include pregnancy and birth control while breast feeding and smoking have been found to be risk factors. It involves all areas in tissues of the joints including tendon, ligament, bone and cartilage. (Figure 1)
Rheumatoid arthritis has a multitude of differential diagnosis including viral polyarthritis, lupus, psoriasis, inflammatory bowel disease, osteoarthritis, gout and CPPD. Lab work and workup including joint aspiration and radiographs of appropriate joints including flexion/extension views of the cervical spine are appropriate. Treatment is primarily conservative with medications including disease modifying anti-rheumatic drugs which have transformed the field and surgery for deformity typically.
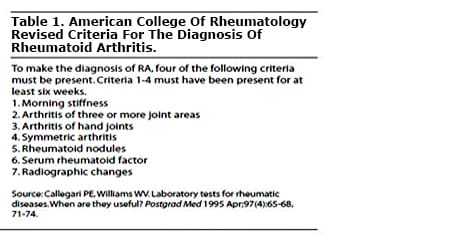
The American College of Rheumatology criteria for diagnosis is noted. (Table 1)
The pathogenesis of rheumatoid arthritis typically involves a Type III hypersensitivity reaction in which immunoglobulins form immune complexes which are then causing an inflammatory response in the joint and affect the synovial lining.(Figure 1) A typical pathologic high powered specimen is viewed with multiple inflammatory cells lining the joint cavity. Typically T lymphocytes and macrophages are involved form a pannus formation which then has a second influx in production of cytokines and multiple chemotactic factors which then cause and induce destruction of all tissues within the joint.
Rheumatoid myelopathy (or spinal cord dysfunction) typically involves atlantoaxial subluxation, or instability between the first two neck bones, (Figure 2) subaxial subluxation (instability or compression below the second neck bone) and basilar invagination, or brainstem compression, (Figure 3) as the presenting radiographic findings. Myelopathy is classified by subjective (patient reported) weakness with abnormal reflexes, objective weakness (on exam), and ambulatory status.
 |
 |
Atlantoaxial instability (FIgure 4) indicates a transverse atlantal ligament disruption which is a contraindication to elective surgeries. The space available for the cord was characterized by Boutin, et al in JVJS, 1992, and when less than thirteen decreased neurologic outcomes are expected. (Figure 5)
 |
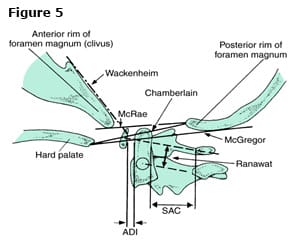 |
Rheumatoid basilar invagination is a settling of the C1 ring or washer on the C2 dens with protrusion past the foramen magnum and compression of the brain stem and neurologic structures.
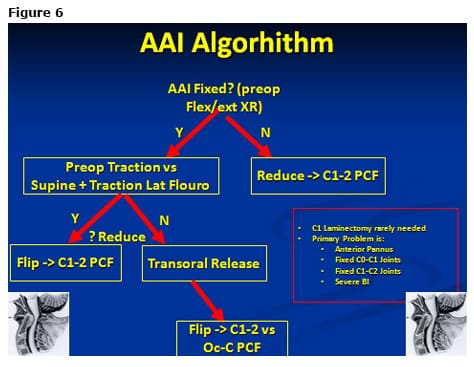
Treatment of rheumatoid arthritis after failure of medical management typically involves a combination of indirect or direct decompression with or without traction via anterior or posterior approaches and a combination of fusion whether that be from C1-2, the skull (occiput) to cervical vertebra or subaxial fusion. The atlantoaxial instability algorithm begins by determining whether or not the deformity is fixed on flexion/extension views. If it is not fixed, then the treatment is reduction and a posterior C1-C2 fusion. If it is fixed, preoperative traction versus supine positioning and intraoperative traction with a lateral fluoroscopy shot will demonstrate a reduction or not. If it does reduce, then you should flip the patient prone and do a C1-C2 posterior fusion. If it does not reduce, a transoral release with rarely an odontoidectomy is indicated and then a prone positioning with a posterior stabilization procedure. Please note, a C1 laminectomy is rarely needed as the primary problem is a combination typically from an anterior pannus, fixed C0-C1 or C1-C2 joints or severe basilar invagination. (Figure 6)
An example case is shown.
Case 1 (Figure 7-8)
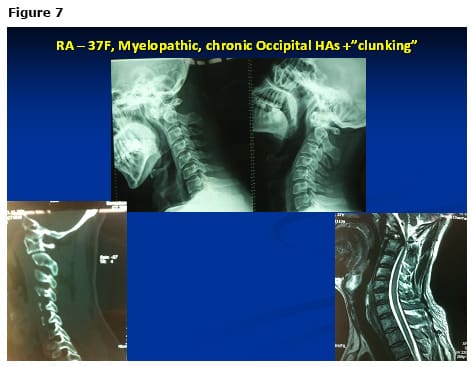 |
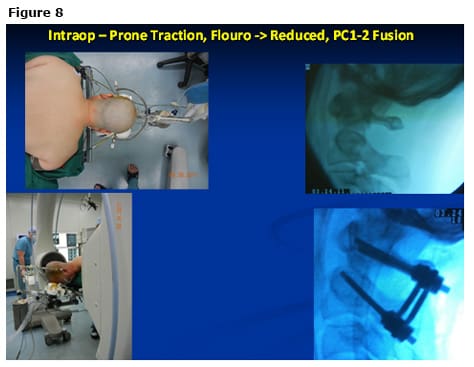 |
Case 2 (Figure 9-10)– A 65-year-old rheumatoid myelopathic with occipital headaches and clunking. X-rays demonstrate a reducible atlantoaxial instability but dynamic cord compression with the space available for the cord of 6.0. However, the large vertebral arteries (going to the back of the brain) are abnormal in the second cervical bone. This patient underwent C1-C2 fusion with bilateral C1 lateral mass screws, as well as C2 translaminar screws.
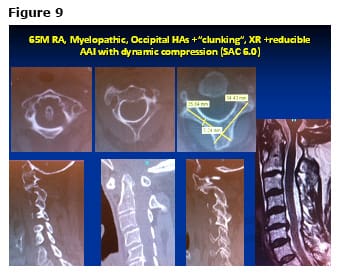 |
 |
In summary, rheumatoid arthritis is much better managed medically than in previous decades due to more potent and better medications with aid of our primary care and rheumatology doctors. However, cervical spinal deformities due still occur regularly that are “different” from typical neck arthritis and require different more advanced surgical techniques.