Spine surgery is traditionally done as “open surgery,” meaning the area being operated on is opened with a long incision to allow the surgeon to view and access the anatomy. In recent years, however, technological advances have allowed more back and neck conditions to be treated with a minimally invasive surgical technique.
Because minimally invasive spine surgery (MISS), does not involve a long incision, it avoids significant damage to the muscles surrounding the spine. In most cases, this results in less pain after surgery and a faster recovery.
Spine surgery is typically recommended only when a period of nonsurgical treatment — such as medications and physical therapy — has not relieved the painful symptoms caused by your back problem. In addition, surgery is only considered if your doctor can pinpoint the exact source of your pain, such as a herniated disk or spinal stenosis.
Minimally invasive techniques are beginning to be used for a wider range of spine procedures, and have been used for common procedures like decompression and spinal fusion since the 1990s. Decompression relieves pressure put on spinal nerves by removing portions of bone or a herniated disk. Spinal fusion corrects problems with the small bones of the spine (vertebrae). The basic idea is to fuse together the painful vertebrae so that they heal into a single, solid bone. This article focuses on decompression and fusion with a minimally invasive technique.
Minimally invasive spine surgery (MISS) is sometimes called less invasive spine surgery. In these procedures, doctors use specialized instruments to access the spine through small incisions.
In a traditional, open surgery, the doctor makes an incision that is 5 to 6 in. long and moves the muscles to the side in order to see the spine. With the muscles pulled to the side, the surgeon can access the spine to remove diseased and damaged bone or intevertebral disks. The surgeon can also easily see to place screws, cages, and any bone graft materials necessary to stabilize the spinal bones and promote healing.
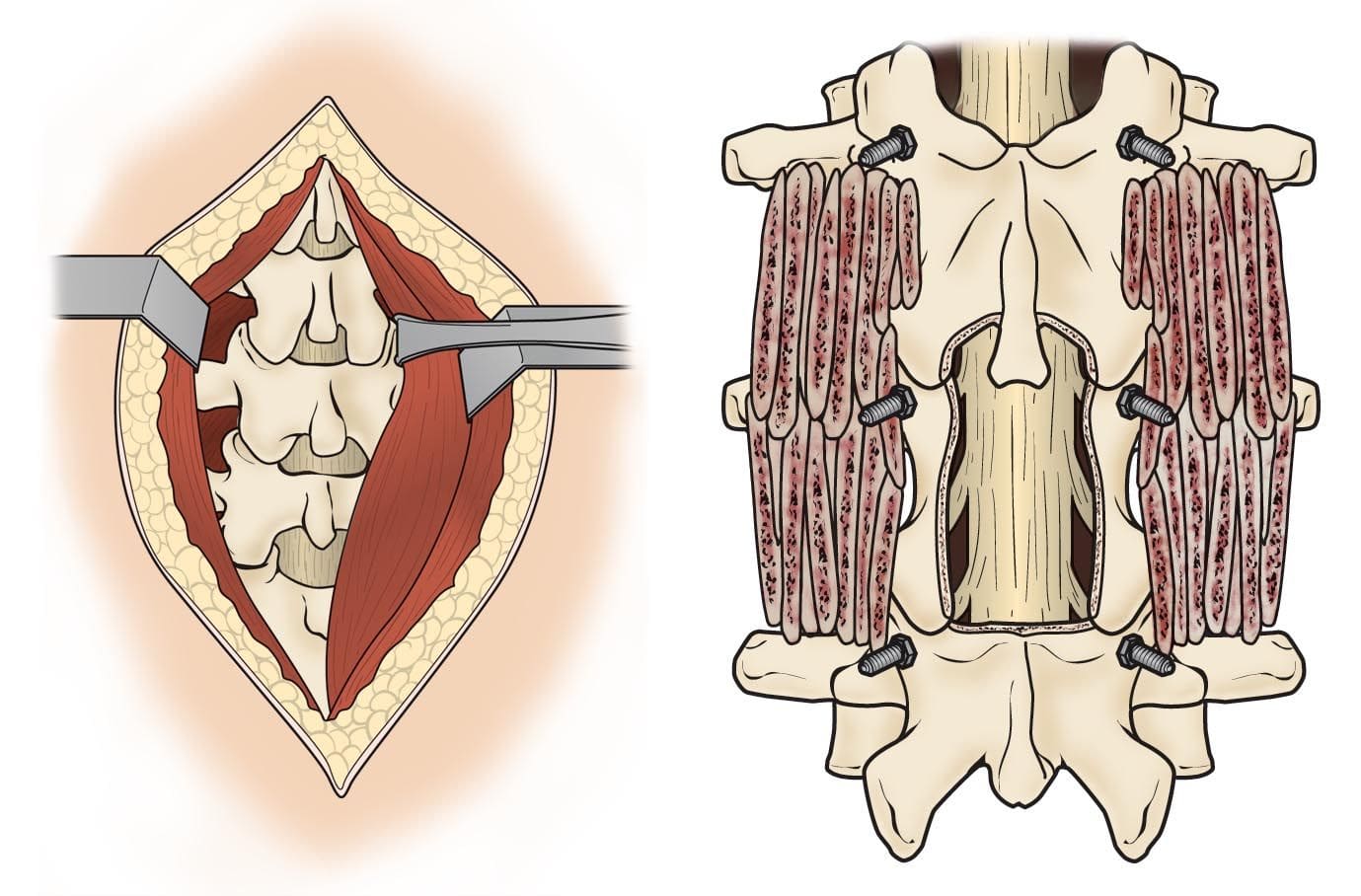
(Left) In open surgery, muscles surrounding the spine are pulled back to reveal the bones. (Right) After removing portions of the bone (a decompression procedure called laminectomy), bone graft material and screws are placed along the sides of the vertebrae.
One of the major drawbacks of open surgery is that the pulling or “retraction” of the muscle can damage the soft tissue. Although the goal of muscle retraction is to help the surgeon see the problem area, it typically affects more anatomy than the surgeon requires. As a result, there is greater potential for muscle injury, and patients may have pain after surgery that is different from the back pain felt before surgery. This can lead to a lengthier recovery period.
Minimally invasive spine surgery was developed to treat spine problems with less injury to the muscles and other normal structures in the spine. It also helps the surgeon to see only where the problem exists in the spine. Other advantages to MISS include smaller incisions, less bleeding, and shorter stays in the hospital.
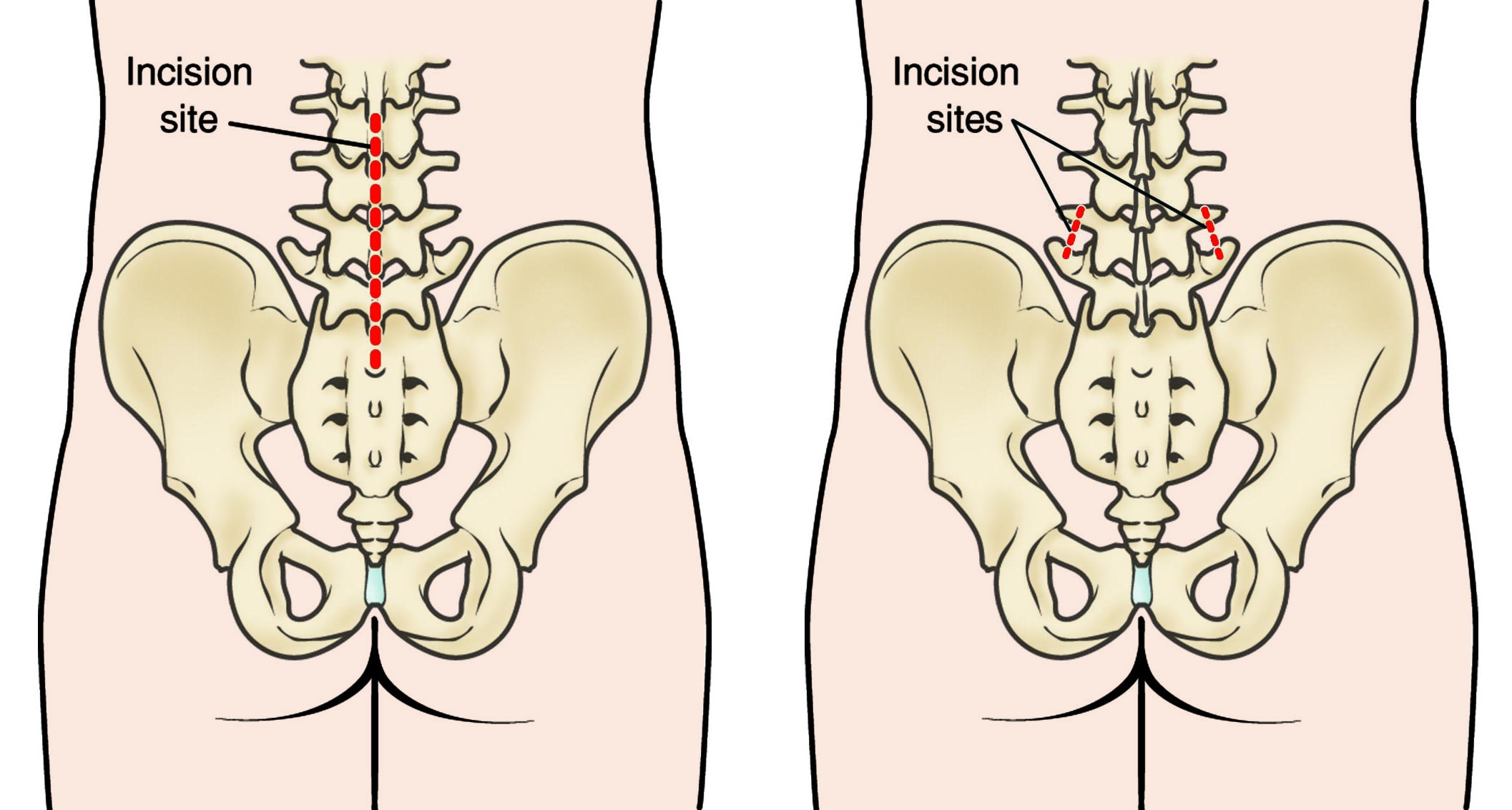
(Left) The incision site in the lower back that is used for some traditional open spine surgeries. (Right)The minimally invasive incisions typically used for a lumbar spinal fusion. Both the decompression and the placing of screws and rods are accomplished through these small incisions.
 Procedure
Procedure
MISS fusions and decompression procedures (such as diskectomy and laminectomy) are performed with special tools called tubular retractors. During the procedure, a small incision is made and the tubular retractor is inserted through the skin and soft tissues down to the spinal column. This creates a tunnel to the small area where the problem exists in the spine. The tubular retractor holds the muscles open and is kept in place throughout the procedure.

A tubular retractor is used to create a passageway for the surgeon to reach the problem area of the lower back.
The surgeon accesses the spine using small instruments that fit through the center of the tubular retractor. Any bone or disk material that is removed exits through the retractor, and any devices necessary for fusion — such as screws or rods — are inserted through the retractor. Some surgeries require more than one retractor.
In order to see where to place the incision and insert the retractor, the surgeon is guided by fluoroscopy. This method displays real-time x-ray images of the patient’s spine on a screen throughout the surgery. The surgeon also uses an operating microscope to magnify the view through the retractor.
At the end of the procedure, the tubular retractor is removed and the muscles return to original position. This limits the muscle damage that is more commonly seen in open surgeries.
The most common types of anesthesia used for MISS are general (you are asleep for the entire operation) and regional (you may be awake but have no feeling from your waist down).
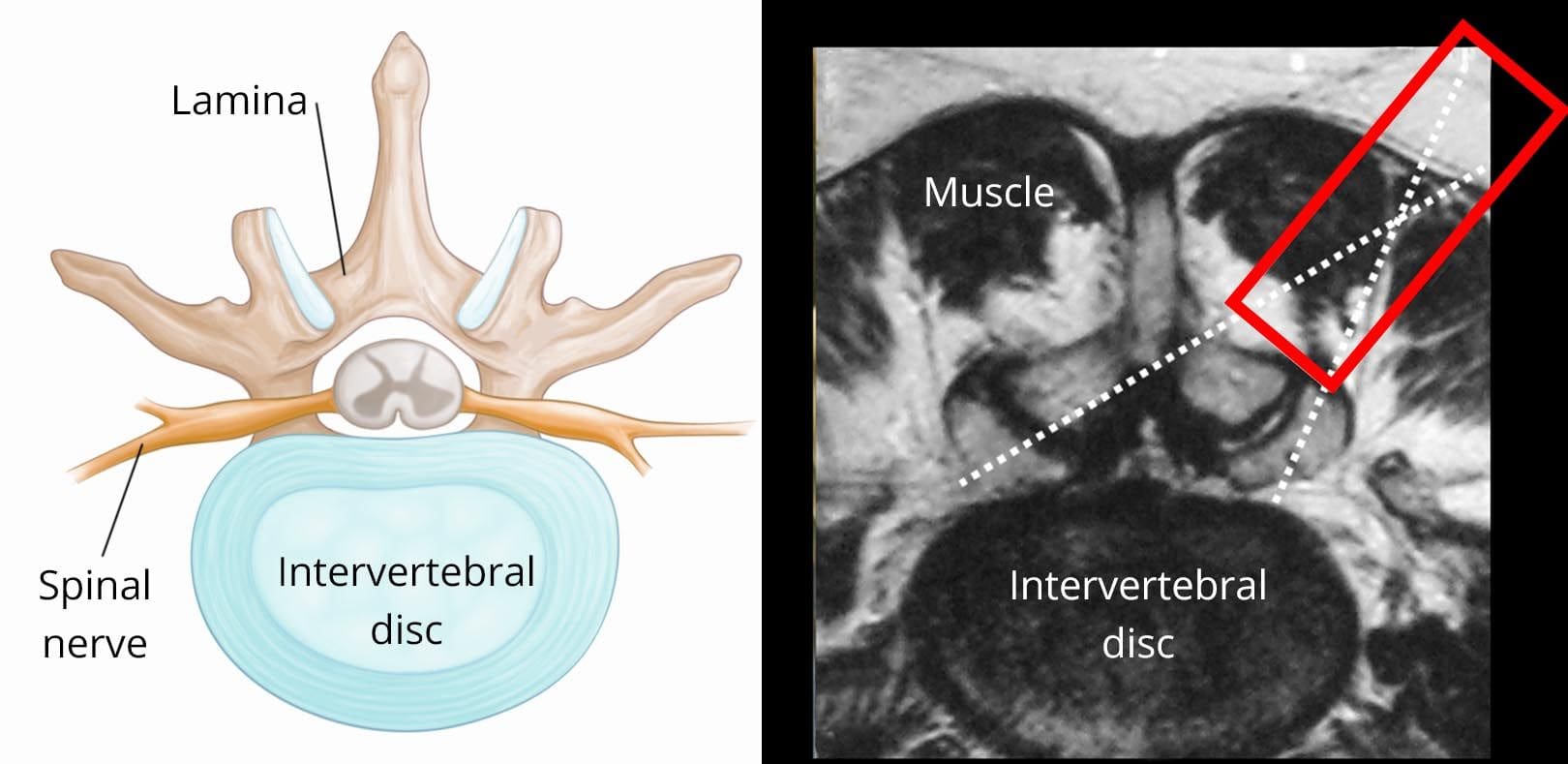
(Left) Cross-section view of a healthy intervertebral disk. (Right) Cross-section MRI scan showing the anatomy surrounding an intervertebral disk. The red rectangle shows placement of the tubular retractor through the muscle. The dotted lines show the positioning of small surgical instruments.
Common Minimally Invasive Spine Surgeries
MIS Lumbar Diskectomy: A herniated disk in the lower back that pinches a nerve may cause severe leg pain, numbness, or weakness. To surgically relieve these symptoms, the disk is removed. This procedure is called a diskectomy.
For the surgery, the patient is positioned face-down and a small incision (sometimes less than 1 in.) is made over the location of the herniated disk. The surgeon inserts the retractor and removes a small amount of the lamina bone. This provides the surgeon with a view of the spinal nerve and the disk. The surgeon carefully retracts the nerve, removes the damaged disk, and replaces it with bone graft material.
This minimally invasive technique can also be used for herniated disks in the neck. The procedure is done through the back of the neck and called an MIS posterior cervical diskectomy.
MIS Lumbar Fusion: A standard, open lumbar fusion may be performed from the back, through the abdomen, or from the side. Minimally invasive lumbar fusions can be done the same way.
A common MISS fusion is the transforaminal lumbar interbody fusion (TLIF) Using this technique, the surgeon approaches the spine a little bit from the side, which reduces how much the spinal nerve must be moved.
In an MIS TLIF, the patient is positioned face-down and the surgeon places one retractor on either side of the spine. This approach prevents disruption of the midline ligaments and bone. Using the two retractors, the surgeon can remove the lamina and the disk, place the bone graft into the disk space, and place screws or rods to provide additional support.
Approaching the spine slightly from the side does not provide the surgeon with a full view and it is often a challenge to remove the disk completely. This may make fusion healing more difficult. Sometimes the surgeon will use additional bone graft besides the patient’s own bone to improve the likelihood of healing.
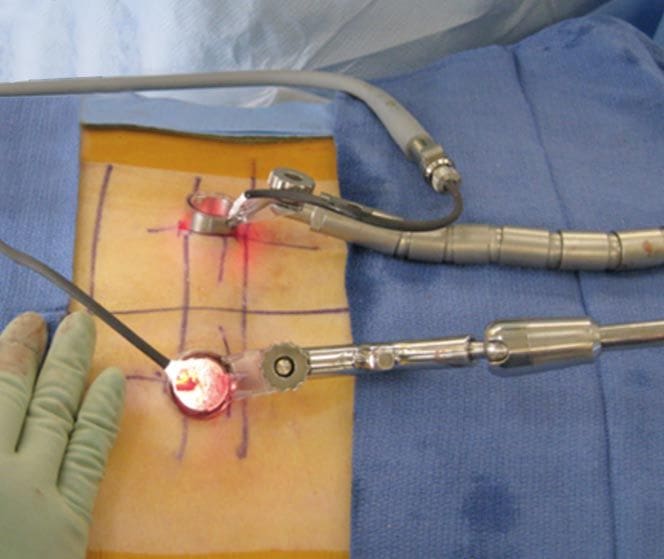
In an MIS TLIF procedure, a tubular retractor is placed on either side of the spine.
Minimally invasive spinal fusion is also commonly performed from the side. There are two procedures that use a side approach: extreme lateral interbody fusion (XLIF) and direct lateral interbody fusion (DLIF). The benefits of these lateral fusion surgeries are that they do not injure the muscles in the back and they do not tug or pull on the nerves in the spinal canal.
Complications
As with any operation, there are potential risks associated with MISS. Complications of MISS are similar to open spinal fusion surgeries, however, some studies show a reduced infection rate for MISS. It is important to discuss these risks with your surgeon before your procedure.
- Infection. Antibiotics are regularly given to the patient before, during, and often after surgery to lessen the risk of infections.
- Bleeding. A certain amount of bleeding is expected, but this is not typically significant.
- Pain at graft site. A small percentage of patients will experience persistent pain at the bone graft site.
- Recurring symptoms. Some patients may experience a recurrence of their original symptoms.
- Pseudarthrosis. Patients who smoke are more likely to develop a pseudarthrosis. This is a condition where there is not enough bone formation. If this occurs, a second surgery may needed in order to obtain a solid fusion.
- Nerve damage. It is possible that the nerves or blood vessels may be injured during these operations. These complications are very rare.
- Blood clots. Another uncommon complication is the formation of blood clots in the legs. These pose significant danger if they break off and travel to the lungs.
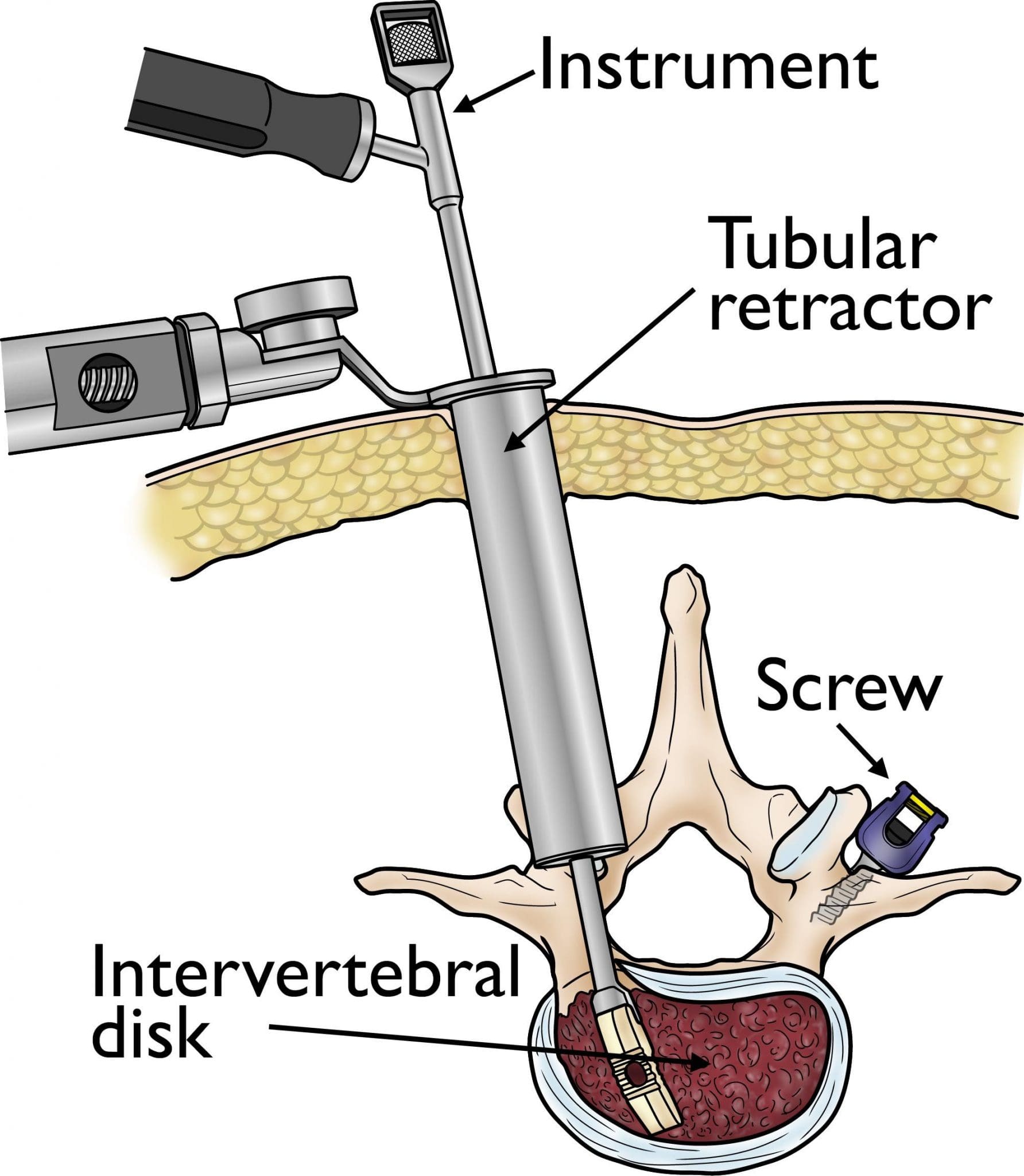
A small instrument is inserted through the tubular retractor to remove a herniated disk. Screws to support the fusion are placed in the bone through both retractors.
Recovery
Minimally invasive procedures can shorten hospital stays. The exact length of time needed in the hospital will vary with each patient and individual procedure, but generally, MISS patients go home in 2 to 3 days.
Because minimally invasive techniques do not disrupt muscles and soft tissues, it is believed that post-operative pain is less than pain after traditional, open procedures. You should still expect to feel some discomfort, however, advancements in pain control now make it easier for your doctor to manage and relieve pain.
To help you regain strength and speed your recovery, your doctor may recommend physical therapy. This will depend on the procedure you have had and your general physical condition. Specific exercises will help you become strong enough to return to work and daily activities.
If you have had a fusion procedure, it may be several months before the bone is solid, although your comfort level will often improve much faster. During this healing time, the fused spine must be kept in proper alignment. You will be taught how to move properly, reposition, sit, stand, and walk.
How long it will take to return to your daily activities after MISS depends upon your individual procedure and condition. Your doctor will evaluate you after your surgery to make sure that your recovery is progressing as expected.
This article is property of American Academy of Orthopedic Surgeons. More helpful information may be found at aaos.org